Abstract
Post-transplant lymphoproliferative disorder (PTLD) following hematopoietic stem cell transplantation (HSCT) is a rare, but life-threatening complication. PTLD typically develops within 6-12 months of HSCT, which is before the reconstitution of EBV-specific cytotoxic T-cell immunity. Several risk factors for developing PTLD have been reported in the literature, including the use of antithymocyte globulin (ATG) and ex vivo T-cell depletion (TCD). However, only a few large-scale retrospective studies have been conducted and risk scores have not yet been well defined. Therefore, to further evaluate the probability of and risk factors for PTLD and establish a risk scoring system, we conducted a retrospective multicenter analysis using data from a Japanese nationwide transplant outcome registry database.
A total of 71,904 patients aged 16 years or older who received HSCT between January 1990 and December 2016 were included in this study. We excluded patients for whom information regarding the transplantation type or PTLD development was unavailable, resulting in 64,539 patients ultimately being analyzed. The probability of developing PTLD was estimated using the Kaplan-Meier method, and differences between groups were evaluated using the log-rank test. To identify risk factors for PTLD, univariate and multivariate analyses were performed using the Cox's proportional hazard regression model for patients who received allogeneic HSCT.
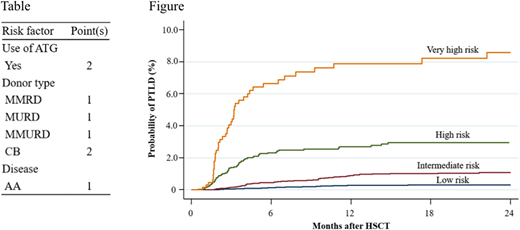
Among the 64,539 patients analyzed, 40,195 received allogeneic HSCT, 24,215 received autologous HSCT, and 129 received syngeneic HSCT. A total of 299 patients developed PTLD, including 267 who had received allogeneic HSCT, 31 who had received autologous HSCT, and one who had received syngeneic HSCT. The median age of patients with PTLD after allogeneic HSCT was 44 years (range, 16-76), and males accounted for approximately 60%. The underlying disease was acute myeloid leukemia and myelodysplastic syndrome in 20,474 patients (51%), acute lymphoblastic leukemia in 6,808 (17%), chronic myeloid leukemia and myeloproliferative disorder in 2,827 (7%), malignant lymphoma in 7,824 (19%), aplastic anemia (AA) in 1,327 (3%) and others in 932 (2%). ATG was used in 4,026 patients (10%) who underwent allogeneic HSCT. In contrast, ex vivo TCD was used only in 296 (0.7%). The donor type was human leukocyte antigen (HLA)-matched-related donor (MRD) in 13,058 patients (33%), HLA-mismatched-related donor (MMRD) in 4,095 (10%), HLA-matched-unrelated donor (MURD) in 10,216 (25%), HLA-mismatched-unrelated donor (MMURD) in 1,993 (5%) and unrelated cord blood (CB) in 10,118 (25%), but was unknown for the remaining 715 patients (2%).The probability of PTLD at 2 years after HSCT was 0.79% with a median onset of 131 (range, 15-6,356) days in patients after allogeneic HSCT. In contrast, the probability of PTLD was 0.11% with a median onset of 198 (range, 21-4,759) days in those after autologous HSCT. Only one patient developed PTLD at 29 days in those after syngeneic HSCT (0.78%). In multivariate analyses performed for patients after allogeneic HSCT, the following variables were identified as risk factors for PTLD: the use of ATG, donor type (MMRD, MURD, MMURD and CB), disease (AA), the number of HSCT, year of HSCT, and acute graft-versus-host disease (grade II-IV). To predict the risk of developing PTLD before HSCT, we established a novel scoring system using three pre-transplant risk factors that correlated with the development of PTLD. We assigned point(s) for the three risk factors by referring to each hazard ratio of the multivariate analysis as shown in the Table. Risk scores were calculated by adding each point(s), and patients were then successfully classified into 4 risk groups: low (score 0-1), intermediate (score 2), high (score 3), and very high risk (score 4-5), with probabilities of PTLD at 2 years after HSCT of 0.3, 1.1, 3.0, and 8.6%, respectively (Figure). Although ex vivo TCD is described as a risk factor for PTLD as well as ATG, it was not identified as a significant risk factor for PTLD in our cohort, probably due to the small number of the affected patients.
This scoring system enables us to predict higher risk patients before HSCT. The close monitoring of EBV-DNA may be beneficial for the early diagnosis of these patients and more rapid initiation of treatment interventions, such as rituximab and EBV-specific cytotoxic T cells.
Mori:Janssen: Honoraria; Novartis Pharma: Research Funding; Taisho Toyama Pharmaceutical Co: Honoraria; CHUGAI: Honoraria; Kyowa Hakko Kirin: Honoraria; MSD: Honoraria; Novartis Pharma: Honoraria; Asahi Kasei: Research Funding; SHIONOGI: Honoraria; Pfizer: Honoraria; Japan Blood Products Organization: Honoraria; Shire Japan: Honoraria; Astella Pharma: Honoraria; Celgene: Honoraria; MSD: Research Funding; Eisai: Honoraria; Ono: Honoraria. Kanda:Nippon-Shinyaku: Research Funding; Chugai: Consultancy, Honoraria, Research Funding; Otsuka: Research Funding; Astellas: Consultancy, Honoraria, Research Funding; Eisai: Consultancy, Honoraria, Research Funding; Dainippon-Sumitomo: Consultancy, Honoraria, Research Funding; Kyowa-Hakko Kirin: Consultancy, Honoraria, Research Funding; Taiho: Research Funding; Pfizer: Research Funding; MSD: Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Asahi-Kasei: Research Funding; Ono: Consultancy, Honoraria, Research Funding; Sanofi: Research Funding; Novartis: Research Funding; Shionogi: Consultancy, Honoraria, Research Funding; Taisho-Toyama: Research Funding; CSL Behring: Research Funding; Tanabe-Mitsubishi: Research Funding; Bristol-Myers Squibb: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Mochida: Consultancy, Honoraria; Alexion: Consultancy, Honoraria; Takara-bio: Consultancy, Honoraria. Tanaka:Pfizer: Honoraria; Otsuka: Honoraria; Bristol-Myers Squibb: Honoraria, Research Funding; Novartis Pharma: Honoraria. Ichinohe:Celgene: Honoraria; Takeda Pharmaceutical Co.: Research Funding; Taiho Pharmaceutical Co.: Research Funding; Zenyaku Kogyo Co.: Research Funding; Mundipharma: Honoraria; Bristol-Myers Squibb: Honoraria; Alexion Pharmaceuticals: Honoraria; MSD: Research Funding; Otsuka Pharmaceutical Co.: Research Funding; Sumitomo Dainippon Pharma Co.: Research Funding; Repertoire Genesis Inc.: Research Funding; JCR Pharmaceuticals: Honoraria; Janssen Pharmaceutical K.K.: Honoraria; Novartis.: Honoraria; Nippon Shinyaku Co.: Research Funding; Pfizer: Research Funding; Ono Pharmaceutical Co.: Research Funding; Kyowa Hakko Kirin Co.: Research Funding; Eisai Co.: Research Funding; CSL Behring: Research Funding; Chugai Pharmaceutical Co.: Research Funding; Astellas Pharma: Research Funding. Suzuki:Celgene: Honoraria; Sawai Pharmaceutical: Honoraria; Ohtsuka: Honoraria; MSD: Research Funding; Meiji Seika Pharma: Honoraria; Takeda Pharmaceuticals: Honoraria; Shionogi: Honoraria; Novartis: Honoraria; Mochida Pharmaceutical: Honoraria; Chugai Pharmaceutical: Honoraria; Kyowa-Hakko Kirin: Honoraria; Bristol-Myers Squibb: Honoraria; Sumitomo Dainippon Pharma: Honoraria; Gilead Sciences: Consultancy; MundiPharma: Consultancy; Jazz Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal